Introduction
Physiotherapy in Hamilton West Mountain & Ancaster for Lower Back
Welcome to Westmount Physiotherapy's patient resource about Posterior Lumbar Fusion.
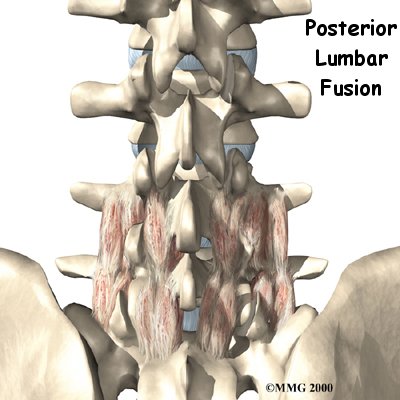
A posterior lumbar fusion is the most common type of fusion surgery for the low back. A fusion is a surgical procedure that joins two or more bones (in this case vertebrae) together into one solid bone. The procedure is called a posterior fusion because the surgeon works on the back, or posterior, of the spine.
Posterior fusion procedures in the lumbar spine are used to treat spine instability, severe degenerative disc disease, and fractures in the lumbar spine.
Other procedures are usually done along with the spinal fusion to take the pressure off nearby nerves. They may include removing bone spurs and injured portions of one or more discs in the low back. Most surgeons also apply metal screws and rods, called instrumentation, to hold the bones securely while they fuse.
This article will help you understand:
- what surgeons hope to achieve
- what happens during the procedure
- what rehabilitation is like after surgery
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Back Pain|limit:15|heading:Hear from some of our patients who we treated for *Back Pain*#
Anatomy
What parts of the back and spine are involved?
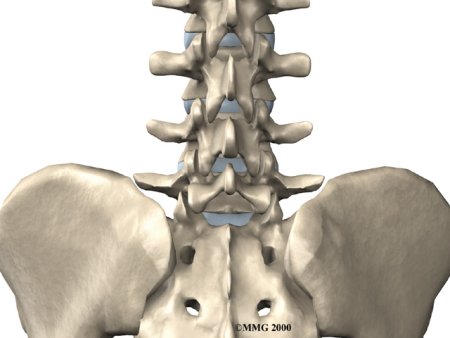
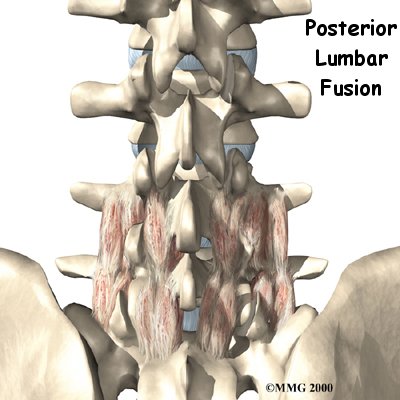
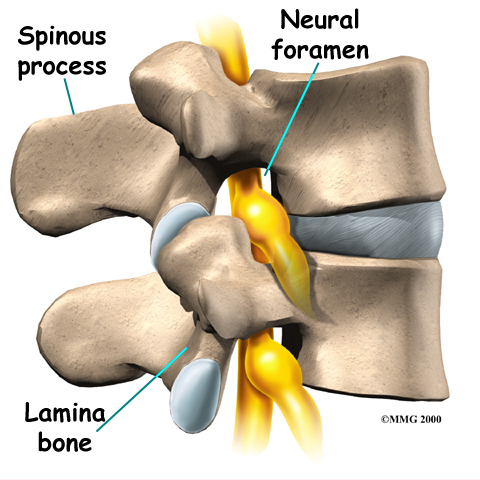
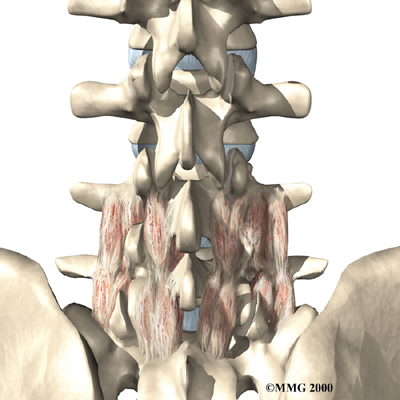
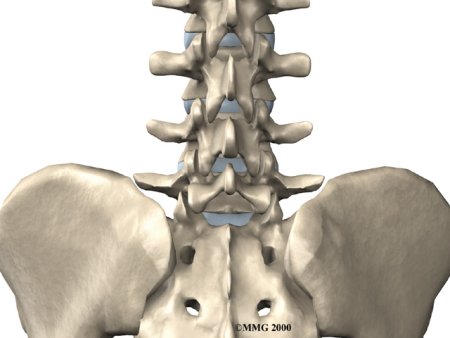
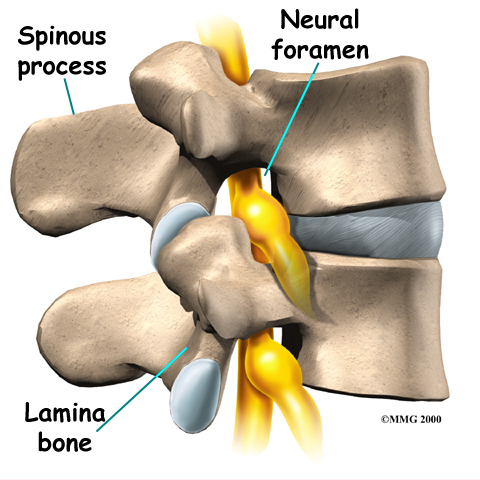
Surgeons perform this procedure through an incision in the low back. The incision reaches to the , the bony projections off the back of the vertebrae. The surgeon must move aside the muscles along the spine, called the paraspinal muscles. The fusion itself involves the lamina bone, the protective roof over the back surface of the spinal cord. In some cases, the surgeon may enlarge the neural foramina, the tunnels where the nerve roots leave the spinal cord.
Related Document: Westmount Physiotherapy's Guide to Lumbar Spine Anatomy
Rationale
What do surgeons hope to achieve?
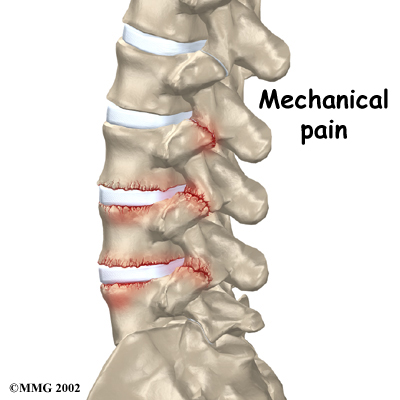
The main goal of the spinal fusion (also known as an arthrodesis) is to stop movement of one or more vertebrae. Keeping the fused section from moving helps stop mechanical pain. Mechanical pain occurs when damaged discs and joints that connect the vertebrae become inflamed from excessive motion between the vertebrae. This type of pain is commonly felt in the low back and may radiate into the buttocks and upper thighs.
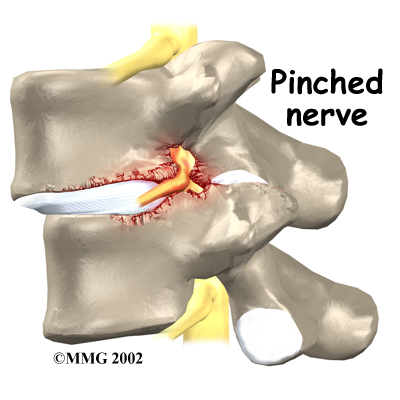
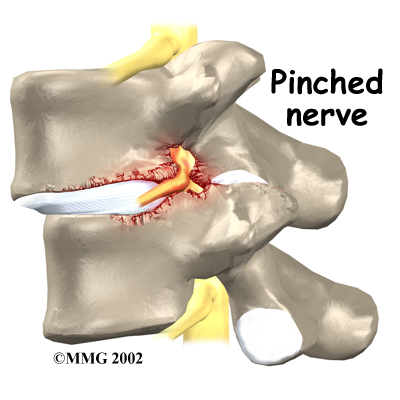
The spinal nerves are also affected by too much vertebral motion. They begin to rub where they pass through the neural foramina and become swollen and irritated. Also, the neural foramina narrow when a vertebra slides too far forward or backward over the vertebra below. This immediately where they pass through the neural foramina. Nerve swelling, irritation, and pinching produce neurogenic pain. This type of pain often radiates down one or both legs below the knee. Fusion stops this harm to the nerves.
By fusing the vertebrae together, surgeons hope to slow down the process of degeneration at the fused segments and prevent future problems.
Preparations
How will I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You should understand as much about the procedure as possible. If you have concerns or questions, talk to your surgeon.
Once you decide on surgery, your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn't eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Patients are given a general anesthesia to put them to sleep during most spine surgeries. As you sleep, your breathing may be assisted with a ventilator. A ventilator is a device that controls and monitors the flow of air to the lungs.
 During surgery the patient usually kneels face down on a special operating table. The special table supports the patient so the abdomen is relaxed and free of pressure. This position lessens blood loss during surgery. It also gives the surgeon more room to work.
During surgery the patient usually kneels face down on a special operating table. The special table supports the patient so the abdomen is relaxed and free of pressure. This position lessens blood loss during surgery. It also gives the surgeon more room to work.
An incision is made down the middle of the low back. The tissues just under the skin are . Then the small muscles along the sides of the low back are lifted off the vertebrae, exposing the back of the spinal column. Next, the surgeon takes an X-ray to make sure that the procedure is being performed on the correct vertebrae.
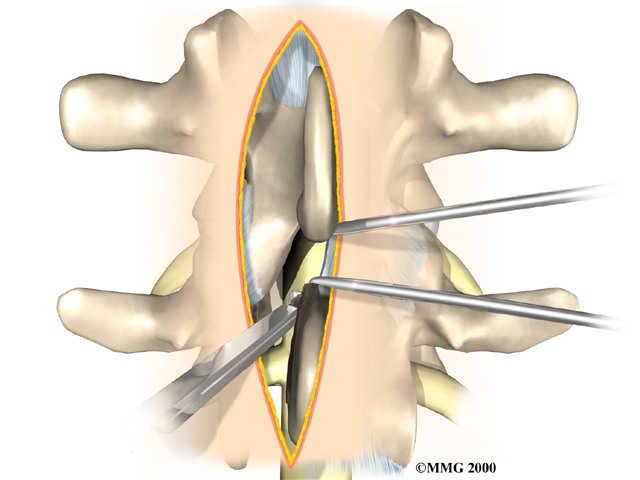
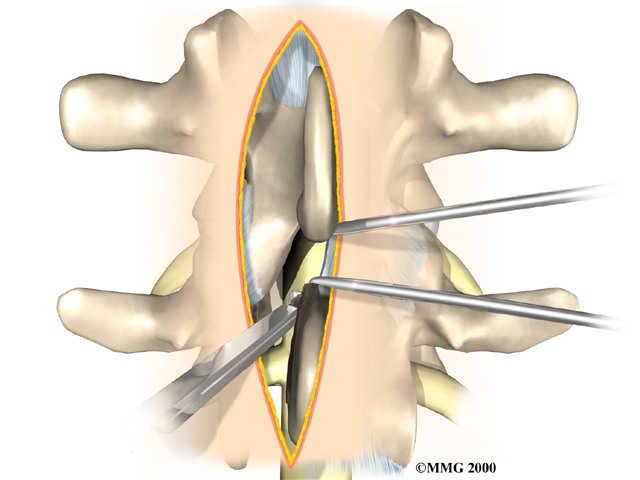
The surgeon first removes any pressure from nearby nerves. This may involve removing part or all of the lamina bone. (The lamina forms the back portion of the bony ring covering the spinal canal.) Then the surgeon takes out any disc fragments and scrapes off nearby bone spurs. In this way, the nerves inside the spinal canal are relieved of additional tension and pressure. The nerve roots are checked to see if they move freely in the spinal canal and as they leave the spine through the small holes between the vertebrae, the neural foramina. If not, the surgeon may cut a larger opening in the neural foramina. This procedure is called foraminotomy.
To prepare the area to be fused, the surgeon shaves a layer of bone off the back surfaces of the spinal column. The cut bone bleeds. The surgeon makes a second incision at the hip. Small strips of bone are removed from the top rim of the pelvis. This is called a bone graft. The surgeon lays the bone strips over the back of the spinal column. When the bone graft contacts the bleeding area, the the bones together just as it would a fractured bone.
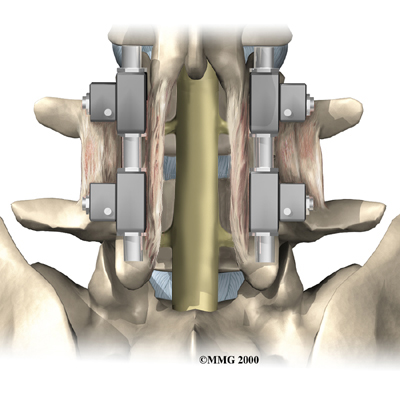
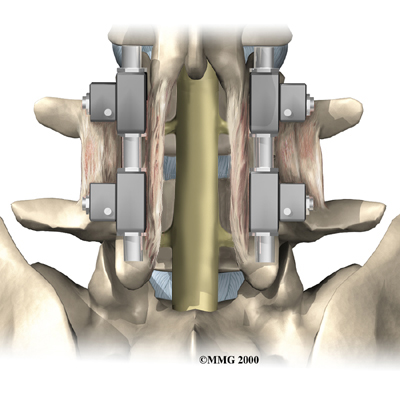
During posterior spinal fusion, the surgeon also fixes the bones in place using a combination of metal screws, rods, and plates. This instrumentation (or hardware, as it is sometimes called) holds the vertebrae to be fused together and prevents them from moving. The less motion there is between two bones trying to heal, the higher the chance they will successfully fuse. The use of instrumentation has increased the success rate of spinal fusions considerably.
A drainage tube may be placed in the wound. The muscles and soft tissues are put back in place, and the skin is stitched together. The surgeon may place you in a rigid brace to support your spine while it heals.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following posterior lumbar fusion include:
- problems with anesthesia
- thrombophlebitis
- infection
- nerve damage
- problems with the graft or hardware
- muscle disruption
- nonunion
- ongoing pain
This is not intended to be a complete list of the possible complications.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include:
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
 Infection
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin's surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat. They may require additional surgery to treat the infected portion of the spine.
Nerve Damage
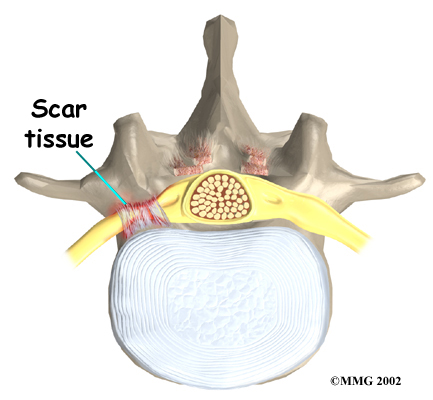
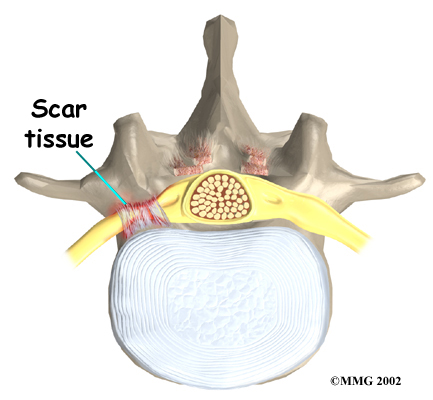
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of . An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
Problems with the Graft or Hardware
Posterior fusion surgery requires bone to be grafted onto the spinal column. The graft is commonly taken from the top rim of the pelvis. There is a risk of pain, infection, or weakness in the area where the graft is taken.
Sometimes the strips of bone graft don't take and end up dissolving. A second surgery may be needed to remove the strips and apply more graft material. The doctor may need to apply additional metal hardware to hold the new grafts firmly in place.
When instrumentation is used, the screws, rods, or plates can also cause problems. They can loosen and irritate the nearby soft tissues. In rare cases, they may actually break. If your hardware loosens or breaks, the surgeon may suggest another surgery either to take out the hardware or to add more hardware to solve the problem.
 Muscle Disruption
Muscle Disruption
During the operation, the surgeon lifts off the small muscles that run along the back of the spinal column. Some of the nerves going to the muscles are cut. Lifting the muscles away from the bone impairs the blood supply to the muscles. Disruption of the nerve and blood supply can cause the muscles to fatigue easily, especially during a long work day and with heavy or repeated lifting. Exercises designed by a physiotherapist boost strength and endurance in the nearby muscles, reducing symptoms from this problem.
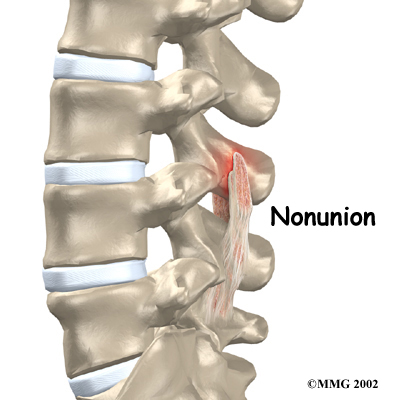
Nonunion
Sometimes the bones do not fuse as planned. This is called a nonunion, or . (The term pseudarthrosis means false joint.) When more than one level of the spine is fused at one time, there is a greater chance that nonunion will occur. Fusion of more than one level means that two or more consecutive discs are removed and replaced with bone graft. If the joint motion from a nonunion causes pain, you may need a second operation.
In the second procedure, the surgeon usually adds more bone graft. Metal plates and screws may also be added to rigidly secure the bones so they will fuse together.
Ongoing Pain
Posterior lumbar fusion is a complex surgery. Not all patients get complete pain relief with this procedure. Successful fusion occurs in more than 80 percent of surgeries. But a solid fusion does not guarantee freedom from pain or the ability to return to normal activity. If you have pain that continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after surgery?
Patients may be placed in a rigid body brace after surgery. This brace may not be needed if the surgeon attached metal hardware to the spine during the surgery. The drain tube is removed from the wound within 24 to 48 hours.
Patients usually stay in the hospital after surgery for up to one week. During this time, a physiotherapist helps patients learn safe ways to move, dress, and do activities without putting extra strain on the back. Patients may be instructed to use a walker for the first day or two. Before going home, patients are shown how to help control pain and avoid problems.
Patients are able to return home when their medical condition is stable. However, they are usually required to keep their activities to a minimum in order to give the graft time to heal. Patients should avoid bending, lifting, twisting, driving, and prolonged sitting for up to six weeks. Outpatient physiotherapy usually starts a minimum of six weeks after surgery.
Patients gradually do more activities and exercise with the goal of getting back to a normal and productive life.
Our Rehabilitation
What should I expect as I recover?
Rehabilitation after posterior lumbar fusion can be a slow process. Although time required for recovery is different for each individual, at Westmount Physiotherapy, our outpatient physiotherapy typically begins a minimum of six weeks after surgery. This delay is needed to make sure the fusion is taking. As a guideline, you will probably need to attend physiotherapy sessions for about two to three months, and should expect full recovery to take up to eight months. Physiotherapy can usually progress faster in patients who had an instrumented fusion.
At first, our treatments are used to help control your pain and inflammation. Ice and electrical stimulation treatments are commonly used to help with these goals. Our physiotherapist may also use massage and other hands-on techniques to ease muscle spasm and pain.
 We will then slowly add active treatments to your therapy program. These include exercises for improving heart and lung function. Short, slow walks are generally safe to start with after posterior lumbar fusion. Swimming and the use of a machine for cardiovascular exercise are helpful in the later phases of treatment. Our therapists also teach patients to help tone and control the muscles that stabilize the low back.
We will then slowly add active treatments to your therapy program. These include exercises for improving heart and lung function. Short, slow walks are generally safe to start with after posterior lumbar fusion. Swimming and the use of a machine for cardiovascular exercise are helpful in the later phases of treatment. Our therapists also teach patients to help tone and control the muscles that stabilize the low back.
Your physiotherapist at Westmount Physiotherapy will work with you on how to move properly and perform certain activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This type of training helps you keep your back in safe positions as you go about your work and daily activities. Training includes positions you use when sitting, lying, standing, and walking. Our physiotherapist will also help you work on safe body mechanics for lifting, carrying, pushing, and pulling.
As your condition improves, we tailor your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires strenuous tasks. Our physiotherapist may suggest changes in job tasks that enable you to go back to your previous employer or to do alternate forms of work. You'll learn to do these tasks in new ways that keep .
Before your physiotherapy sessions end, our physiotherapist will teach you how to avoid future problems.
Westmount Physiotherapy provides services for physiotherapy in Hamilton West Mountain & Ancaster.
Portions of this document copyright MMG, LLC.








 During surgery the patient usually kneels face down on a special operating table. The special table supports the patient so the abdomen is relaxed and free of pressure. This position lessens blood loss during surgery. It also gives the surgeon more room to work.
During surgery the patient usually kneels face down on a special operating table. The special table supports the patient so the abdomen is relaxed and free of pressure. This position lessens blood loss during surgery. It also gives the surgeon more room to work.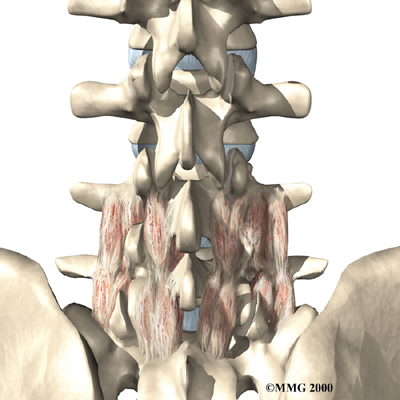
 Infection
Infection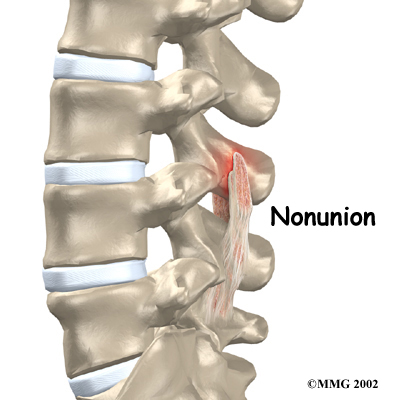 Muscle Disruption
Muscle Disruption We will then slowly add active treatments to your therapy program. These include exercises for improving heart and lung function. Short, slow walks are generally safe to start with after posterior lumbar fusion. Swimming and the use of a machine for cardiovascular exercise are helpful in the later phases of treatment. Our therapists also teach patients
We will then slowly add active treatments to your therapy program. These include exercises for improving heart and lung function. Short, slow walks are generally safe to start with after posterior lumbar fusion. Swimming and the use of a machine for cardiovascular exercise are helpful in the later phases of treatment. Our therapists also teach patients